How has MARS been developed?
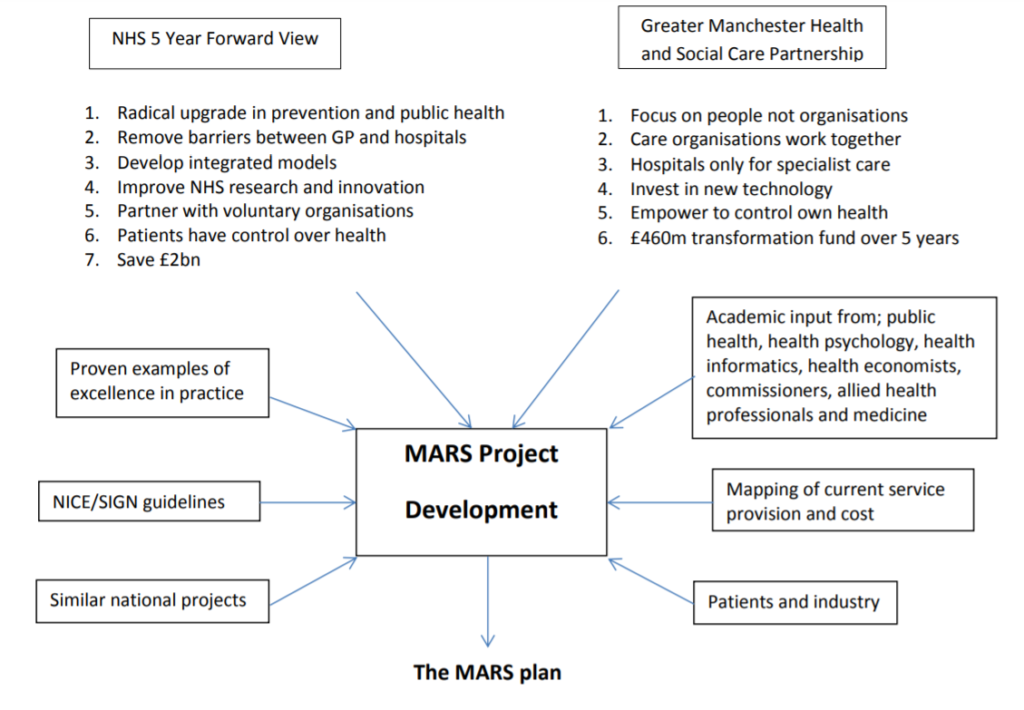
The MARS Project has brought together over 40 regional and national stakeholders spanning the health economy and is already adapting an innovative IT solution. MARS has been developed following close consultation with commissioners, health professionals, academics and industry adhering to the principles of transformation set out in the NHS forward view and Devolution Manchester documents.
One of the key stakeholders supporting the development of the MARS project is the Greater Manchester Strategic Clinical Network (SCN) part of the Greater Manchester Health and Social Care Partnership. The SCN has published a number of documents which incorporate lower limb guidelines: the GM Diabetes Clinical Best Practice Strategy, which describes the need for rapid access to lower limb services through a co-ordinated integrated lower limb pathway across GM; the STAMP (STop unnecessary AMPutations) pathway commissioned to improve the management of people presenting with Critical Limb Ischaemia across Greater Manchester, Eastern Cheshire and Lancashire; and the Assessment, Diagnosis and Management of People at Risk of Lower Limb amputation.
What is the MARS plan?
The MARS plan is based on the principle that an amputation is the culmination of a number of steps and therefore each phase, in the iceberg of disease, leading to an amputation requires an intervention. It is equally important to improve care and reduce costs by both preventing and aggressively healing chronic ulcers.
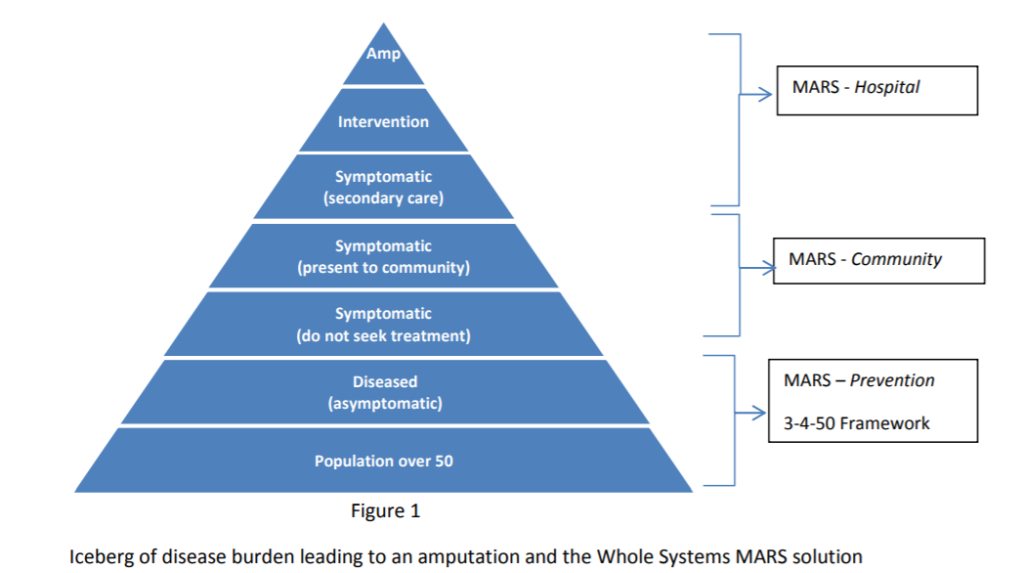
MARS Public Health Framework –The 3-4-50 Strategy and Social Care
Prevention is the key to improving patient outcomes and reducing treatment costs. There are approximately 2.8 million people living in GM of whom 33.2% are aged 50 and over. This population of around one million will be the target of the MARS Public Health Framework. Within this population, 330 000 have the chronic diseases that potentially lead to a chronic wound and amputation and will require a more targeted and personalised approach to preventing amputations.
The aim of the Framework is to co-ordinate prevention initiatives using the 3-4-50 strategy principle that 3 lifestyle behaviours (poor diet, lack of exercise and smoking), lead to 4 health conditions (cardiovascular disease, respiratory disease, Type 2 diabetes and cancer) which lead to 50% of deaths.
The MARS Public Health Framework will complement the Greater Manchester Population Health Plan 2017-21 (www.gmhsc.org.uk/assets/GM-Population-Health-Plan-Full-Plan.pdf). The Plan highlights the importance of poor diet, exercise and smoking as modifiable risk factors to improve population health. These plans will include the role of schools and colleges in encouraging children to develop healthy lifestyles. The plan recognises that change happens in communities, supported
by local organisations. The development of a MARS Public Health Framework will contribute to the achievement of the population health plan objectives. Targeted health promotion messages will be additionally delivered to patients throughout the MARS pathway utilising appropriate technology and multi-disciplinary staff.
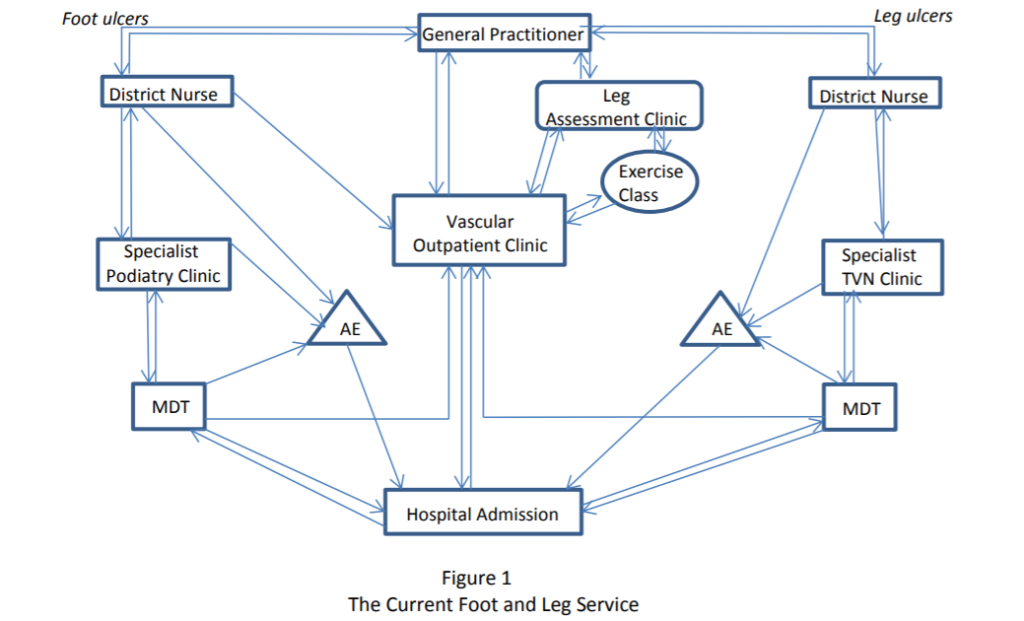
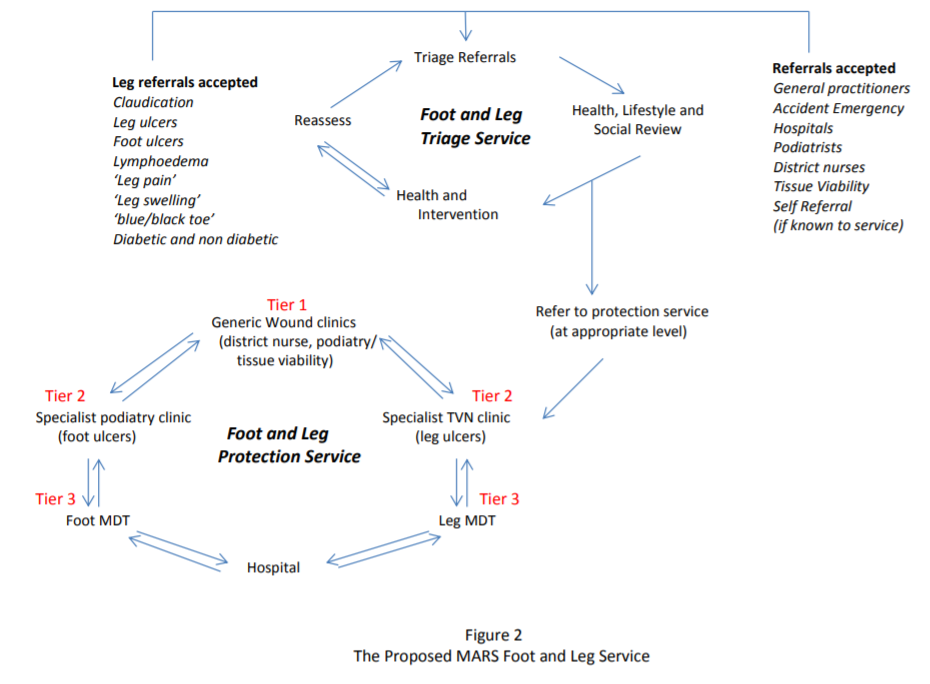
What will the new integrated service look like? (Figures 1 and 2)
MARS aims to reduce the heterogeneity of service provision surrounding community foot and leg ulcer management. The current multiple referral pathways are summarised in figure 1. The proposed MARS pathway is shown in figure 2.
The new pathway will have two components; a ‘Triage Service’ and a ‘Protection Service’. The Triage Service will triage, diagnose and treat the population at risk. It will undertake a health and social care needs assessment. In line with the MARS Public Health Framework the triage service will offer lifestyle and risk factor modification programs and be the centre for health promotion in the community for this high risk population. Patients with foot and leg ulcers will be referred to the Protection Service. Here, there will be three tiers of management; tier 1 (district nurse level) will
manage the most basic of wounds, tier 2 (specialist clinics) will be run by specialist podiatrists and tissue viability nurses with the most complex wounds managed at the multi-disciplinary level (tier 3). Tier 1 and 2 will be in the community and tier 3 in hospital outpatient setting. Patients will move through the tiers seamlessly as the wounds change.
Experienced staff will also rotate through all the tiers in order to support, spread confidence and improve equality in management.
A Practical Example of How the Service May Work
(a non app based system is also envisaged for patients)
 Paul, a 52 year old Engineer, has a poor diet, is overweight and has diabetes. He is also a heavy smoker and drinker. He rarely gets out, has very limited family support and relies on a close circle of friends to offer emotional support. Psychologically he is low. He has recently started to get ulcers on his foot. He is not known to MARS.
Paul, a 52 year old Engineer, has a poor diet, is overweight and has diabetes. He is also a heavy smoker and drinker. He rarely gets out, has very limited family support and relies on a close circle of friends to offer emotional support. Psychologically he is low. He has recently started to get ulcers on his foot. He is not known to MARS.
Paul searches for ‘foot sore / ulcers’ on the internet to try and find out more information and what he can do to help himself. He is worried about the credibility of the information he will find, however he is delighted to see a very specific advert within his search results from the NHS on his condition.
He clicks on the link, which takes him to a website with information on sores and best practice guidance on a number of different areas, such as diet and exercise. Paul also has access to ‘Norman’ the MARS chatbot for foot and leg sores – he can use this online service to ask as many questions as he likes about his condition – he knows he is talking to a computer program, but he likes the anonymity of it. Norman ends up suggesting he see his local GP in Beswick, which is only 1 mile away from his current location – Norman provides contact details for this GP.
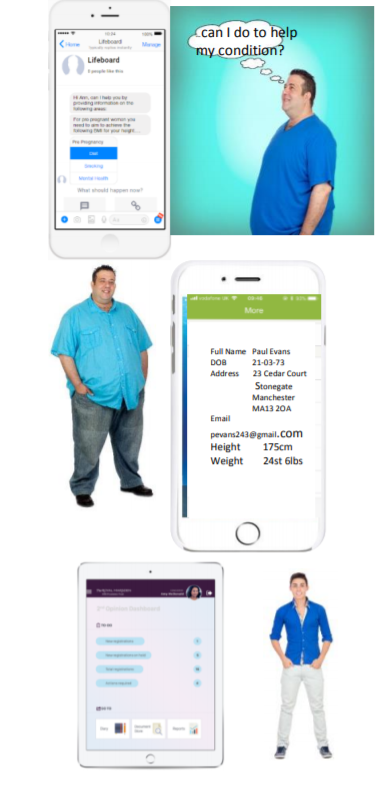 Paul visits his GP who takes some pictures and sends them, along with the usual referral information, to a healthcare professional at MARS. This triggers an email to Paul, allowing him to download the MARS app.
Paul visits his GP who takes some pictures and sends them, along with the usual referral information, to a healthcare professional at MARS. This triggers an email to Paul, allowing him to download the MARS app.
After setting up an account he is pleased to see his GP photos and information already pre-populated. He adds more information to his profile, including height, weight and blood group, plus answers some simple life style questions. If he thinks his condition is getting worse, he can even take photos and send them through to a MARS healthcare professional for review.
Meanwhile, Mike a MARS healthcare professional is alerted to this new support request in his dashboard and reviews the content, in particular the photos – he believes that the ulcers are not too serious, but would like a podiatrist at his local clinic to see him. He adds Sarah, a podiatrist at a local clinic in Beswick, to the collaboration space. Sarah messages Paul with the next available slot – April 24th @ 10am. Paul accepts.
Paul meets Sarah for his appointment and she conducts a full new patient assessment to ‘get it right 1st time’. This includes an assessment and photo of the wound, initiating treatment and review cycles and instigating any investigations required. In short, she educates Paul on how to treat his
 condition, sets up weekly review appointments with a district nurse, books him a session with a social carer (to discuss his diet and weight) and a mental health specialist (at the local clinic). All appointment details are visible in the ‘My appointments’ section of his app. He even gets reminder notifications.
condition, sets up weekly review appointments with a district nurse, books him a session with a social carer (to discuss his diet and weight) and a mental health specialist (at the local clinic). All appointment details are visible in the ‘My appointments’ section of his app. He even gets reminder notifications.
Social Care is notified at the same time as Paul, and is given ‘contributor’ status, which means they can access certain information and capabilities. For example, they use the chat capability in the app to remind Paul that he must complete a preappointment questionnaire in the app.
Paul arrives on time to meet Sally, his social carer. She already has access to his information via her portal. They have a good discussion on his general health and lifestyle and they agree a programme of actions to improve his diet and weight. Immediately after the appointment Paul reviews the various services on offer in the Manchester area, via his app, which could benefit him – these services are personalized to his condition.
Over the coming 2 weeks, Paul has weekly reviews with the district nurse who takes photos of the wound and measures its depth, width and length at each visit – both the photo and measurements are visible on Paul’s mobile.
Paul can see his wound getting worse via the barometer, which tells him the chance of his wound healing in 4 weeks is now 30% based on the most recent photo and measurements. He also thinks his wound has got worse in the past few days, so he decides to take a photo and uploads it via his app. Within the hour, Mike sets an emergency appointment with Sarah for the following day. Sarah sees him and refers him to MARS to get admitted to hospital. Mike, as the ultimately owner of the collaboration space, has access to all of Paul’s details and notes. He messages Paul with an admissions time for the same day, Paul agrees and the ‘Admission’ is put in his ‘My Appointment’ section.
How will MARS achieve this service re-design?
Phase 1 of MARS requires a ‘whole systems analysis’ and will lead to ‘population based
transformation’ through a ‘deep dive’ service review. Phase 2 i.e. implementation will be based on a cost benefit analysis where the focus of the new service will be prevention, early diagnosis and consistent high quality standardised treatment of wounds with improved healing rates.
Phase 1
a) Map current wound care service provision, patient journeys and resources in each locality
b) Develop protocols for community chronic wound treatment for foot and leg ulcers
c) Develop a ‘community wound care team’ model to include non-medical consultant
management
d) Develop an integrated service provision model to ensure seamless pathways between
community and hospital teams
e) Map new MARS pathway and changes required in each locality for its implementation
f) Develop an IT system that facilitates referral across GM using images of wounds
g) Develop a MARS Public Health Framework (3-4-50 strategy)
h) Cost benefit analysis of MARS implementation
i) Develop an implementation strategy for the commissioning of MARS
j) Sign off for MARS service model, Framework and pathway
Phase 2
a) MARS staged implementation
b) Evaluation
What is the timeframe and proposed milestones for Phase 1?
1. Identify and consult regional and national wound care experts January 2017
2. Complete MARS consultation document March 2018
3. Raise MARS profile and apply for funding April 2018
4. Secure funding and launch MARS April 2019
5. Deliver locality specific commissioning strategy April 2021
6. Begin phased implementation of MARS (Phase 2) April 2021
7. Complete MARS implementation April 2023
8. Breakdown of MARS Phase 1 (April 2019-April 2021)
Month 1-3: Formal recruitment of MARS team and executive leaders (already engaged)
Month 2-12: Development of foot ulcer and leg ulcer treatment algorithms
Month 6-18: Locality gap analysis against service model
Month 18-20: Cost Benefit Analysis of MARS Implementation Strategy
Month 20-24: Writing up of final report: Costed MARS Implementation Strategy
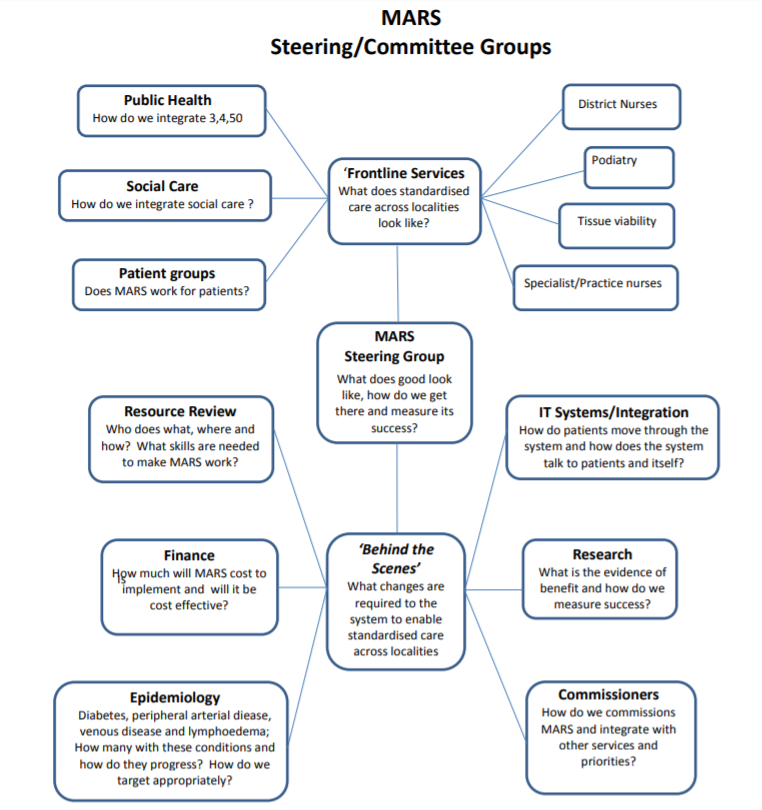
What is the proposed MARS network structure?